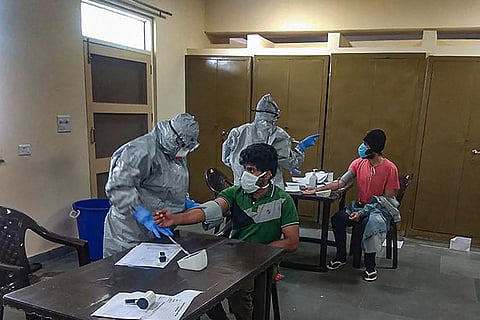
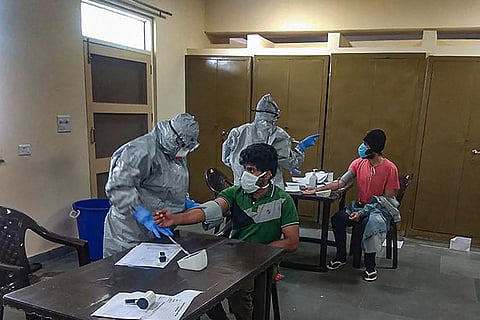
On Tuesday, Dr Jeevan* was placed on duty at the isolation ward for COVID-19 suspected cases, where he was to monitor patients for complaints through the night.
The young medical officer who was posted on COVID-19 duty in a district hospital had been routinely handling swab tests, isolation and monitoring of cases at the hospital, ever since the outbreak of the virus in Kerala.
The (PPE) Kit arrived without a key component - the N95 respirator. The mask, scientifically termed the N95 filtering face mask respirator (FFR) is the life saver component of any personal protective equipment kit.
However, ever since the outbreak of the COVID-19 pandemic, these masks are in acute shortage globally, and Kerala’s medicos too have now begun to face the brunt of a depleting stock of masks.
“I frantically asked my colleagues and searched the hospital to see if I could get hold of one mask before I entered the isolation room which has at least 20 suspected cases. I had only received a triple layer mask with my kit and firmly stated that I will not enter the ward without an N95 mask. Finally, an emergency N95 respirator was somehow arranged for me to enter the ward,” Dr Jeevan recalled to TNM.
Over the last week, news reports have highlighted the shortage of N95 masks and gloves in government hospitals in Kerala, which have forced nurses, nursing assistants and other health care staff to compromise personal safety and discharge their duties.
“Some of the nurses had to use N90 pollution masks inside the isolation ward for a few days. These are not effective in filtering out viruses. And these nurses and nursing assistants who have to administer medicines and injections, tend to the patients in close proximity,” Dr Jeevan added. The issue, he added, has been raised by the hospital and the government had resolved it within a day.
In Tuesday’s meeting with the press, Chief Minister Pinarayi Vijayan claimed that Kerala did not face a scarcity of masks anymore. The state has now decided to put PPE kits to judicious use, distributing them only on a priority basis and in the meantime, attempting to procure more kits from private distributors through the Kerala State Government Medical Supplies Corporation (KGMSC), which handles PPE distribution.
TNM spoke to stakeholders in Kerala’s response teams to get a clearer picture on the availability or shortage of PPE kits.
Not equipped with PPE kits in case of community spread
“As of now we are seeing only a small pool of people - less than 40 cases - testing positive per day. If this situation prevails, then Kerala may not face an acute shortage of kits in the near future. But we will not have enough kits if we see a spike in numbers or community spread. And we need to prepare for any eventuality,” says Dr KS Vijayakrishnan, state secretary of Kerala Government Medical Officers Association (KGMOA).
The kit, including the gloves, gown and the mask are single-use items which cannot be worn for more than four hours at a time. Its disposable nature adds to its acute demand in hospitals when cases increase, he says.
“In every isolation ward, a minimum number of people require PPE kits. This is the doctor, the nurse and the nursing assistant who interact with positive patients or suspected cases. And the cleaner who cleans the bed and room. Further ambulance drivers who transport positive patients and swab samples of suspected cases are also mandated to wear hazmat suits and masks. With more staff entering the isolation room and more patients tested, so many more kits are used up and disposed of,” he explains.
Moreover, in the time that a health worker is in a PPE suit, he cannot perform ordinary functions such as drinking water, eating food or urinating. For this reason, no staff is allowed to stay in a suit and inside the isolation ward beyond four hours.
Open market supply of N95 masks could have also contributed to shortage
Apart from a manufacturing lull and a global rise in demand of personal protective equipment, the surge in open market sales of these components, especially N95 respirators, have contributed to the scarcity, says Father Simon Pallupetta, health secretary of the Kerala Catholic Bishop Council (KCBC).
KCBC had recently promised to offer its hospitals to the Kerala government to combat COVID-19 in the state, when such a need arises. However, most of its hospitals do not yet have stocks of PPE kits.
“You see so many people walking on the roads and riding bikes wearing N95 masks. They are not high risk people in terms of exposure and they do not need to wear them unless there is community spread. These masks should be given to health care workers who interact with positive and suspected cases of coronavirus everyday,” Father Simon adds.
Even as people purchase and use N95 masks everyday, several health care workers in many states have only been able to access basic protection while interacting with home quarantined patients and undiagnosed cases. Kerala has already reported three cases of health care workers contracting the virus, while monitoring home quarantined cases in their districts.
Further, incorrect use of these masks by people also negates any benefit that wearing them might have brought about, Fr Simon observes.
“You can see many people, especially people at airports, wearing surgical masks that are days old. Be it N95 masks or three layer masks, they are supposed to be disposed off after 4-6 hours. Otherwise, the wearer comes in contact with the germs accumulated in the mask, when he or she removes it in order to eat or drink water,” he added.
Private hospitals have zero stocks of PPE kits
Though government hospitals have just about enough kits to handle a small rise in positive cases per day, private hospitals who are setting up ventilators and isolation wards as contingency, have zero PPE stocks.
“We are setting up all the facilities to treat positive patients for when the need arises. However, we do not have enough COVID-19 PPE kits. Just like how accidents kits are not procured after accidents cases arrive, COVID-19 kits too should be stocked up in advance. The government, of course, is looking into procuring more kits,” Fr Simon added.
Stating that most components of these kits are made in China, Taiwan and South Korea, Fr Simon observed that the travel ban to contain the virus and hike in demand also possibly intensified the shortage.
With the 21-day-lockdown imposed by the Centre to flatten the curve of the epidemic, the states now have more time to prepare themselves in case of a community spread, adds Dr Vijayakrishnan.
“The centre has banned the export of protective equipment products and raw material used to manufacture them. The prices of these kits have also been regulated and this helps hospitals where demand is high. Hopefully, we are also able to use this time to secure more kits,” he added.