The world of science and medicine received news of an astounding breakthrough on Tuesday morning. According to reports, a man from London has allegedly been cured of HIV after receiving stem cell transplants from donors who carried a rare genetic mutation, which made them resistant to the virus.
This was the second time that such a case has been documented. In 2008, a man from Berlin, who was undergoing treatment for leukaemia, was cured of HIV after receiving a bone marrow transplant.
Indian-origin scientist and professor Ravindra Gupta from the Infection and Immunity Department of the University College London was the lead author of the study. “By achieving remission in a second patient using a similar approach, we have shown that the Berlin patient was not an anomaly and that it was the treatment approaches that eliminated HIV in these two people,” he said to the media.
Case 1: The Berlin patient
Timothy Ray Brown, a resident of Seattle in Washington, USA, had contracted Human Immunodeficiency Virus (HIV) in 1995 and had been taking antiretroviral (ARV) medications for 11 years. In 2006, he was diagnosed with acute myeloid leukaemia (AML) and had to undergo chemotherapy for the treatment. Timothy was living in Berlin at the time, and after the chemotherapy failed, doctors in Berlin suggested a bone marrow transplant.
A bone marrow transplant is carried out for patients with leukaemia, in cases where deemed necessary. He underwent two transplants and stopped taking his ARVs. Normally, when an HIV-infected person stops taking ARVs, there is a significant surge in the levels of the HIV (virus) present in their blood.
Researchers noticed in Timothy’s case in the past seven years is that only traces of the viral genetic material were found, none of which seemed to be able to replicate.
Doctors monitored Timothy for seven years from 2008 and noticed that only traces of the viral genetic material of HIV were found in his body, none of which were capable of replicating.
Researchers discovered that the bone marrow donor had a unique genetic mutation called CCR5 delta 32, which made his blood cells immune to HIV and thereby preventing the entry of the virus.
Since then, several have tried to replicate the results but to no avail, until now.
Case 2: The London patient
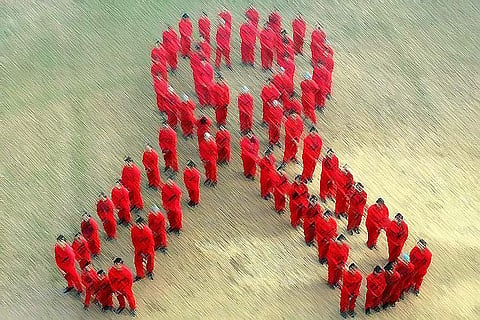
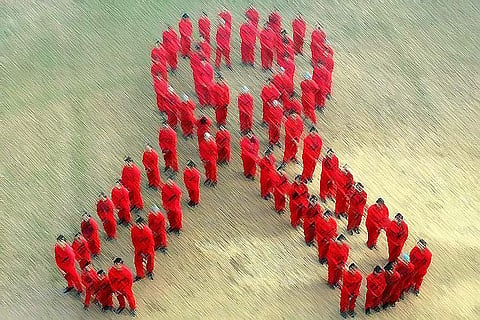
The human immunodeficiency virus (HIV) can be transmitted in several ways. Infected needles, blood and blood particles (in rare cases), sexual contact are some of the primary ways this occurs. When an individual is infected with HIV, the virus starts replicating in the body and begins to attack their immune system. Eventually, the immune system becomes so weakened that it develops AIDS (Acquired Immuno Deficiency Syndrome).
When there is a full-blown onset of AIDS, the person’s immune system cannot defend itself even against some of the most common diseases and infections, the result of which people usually succumb.
When Antiretroviral (ARV) medicines are administered to HIV patients, which it helps keep the virus at bay. These drugs essentially suppress HIV infection but cannot get rid of the virus entirely.
The London patient was started on ARV in 2012, after he was diagnosed with the infection years prior. He was diagnosed with Hodgkins’s lymphoma and underwent a stem cell transplants in 2016 and was continued on ARVs for 16 months. Doctors have been monitoring him since and noticed that the virus has been in remission in this patient’s case for nearly 18 months, that is, hardly any traces of the HIV virus were found in his body.
Dr Pradeep of YRG Care Hospital in Chennai, which works with HIV/AIDS patients, however, says this treatment cannot be considered a cure.
“The two individuals developed an aggressive malignancy, which left the doctors with no choice but to facilitate a bone marrow transplant. And since they knew that certain individuals with a genetic mutation that made them less vulnerable to HIV/AIDS, they used the bone marrow of such individuals to potentially “cure” the virus,” he explained.